For the first time ever, stem cells from umbilical cords have been converted into other types of cells, which may eventually lead to new treatment options for spinal cord injuries and multiple sclerosis, among other nervous system diseases.
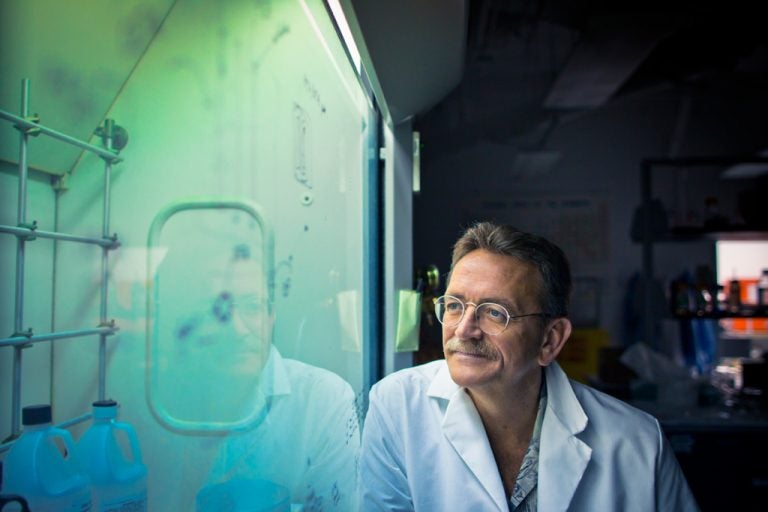
“This is the first time this has been done with non-embryonic stem cells,” says James Hickman, a University of Central Florida bioengineer and leader of the research group, whose accomplishment is described in the Jan. 18 issue of the journal ACS Chemical Neuroscience.
“We’re very excited about where this could lead because it overcomes many of the obstacles present with embryonic stem cells.”
Stem cells from umbilical cords do not pose an ethical dilemma because the cells come from a source that would otherwise be discarded. Another major benefit is that umbilical cells generally have not been found to cause immune reactions, which would simplify their potential use in medical treatments.
The pharmaceutical company Geron, based in Menlo Park, Calif., developed a treatment for spinal cord repair based on embryonic stem cells, but it took the company 18 months to get approval from the FDA for human trials due in large part to the ethical and public concerns tied to human embryonic stem cell research. This and other problems recently led to the company shutting down its embryonic stem cell division, highlighting the need for other alternatives.
Sensitive Cells
The main challenge in working with stem cells is figuring out the chemical or other triggers that will convince them to convert into a desired cell type. When the new paper’s lead author, Hedvika Davis, a postdoctoral researcher in Hickman’s lab, set out to transform umbilical stem cells into oligodendrocytes–critical structural cells that insulate nerves in the brain and spinal cord–she looked for clues from past research.
Davis learned that other research groups had found components on oligodendrocytes that bind with the hormone norephinephrine, suggesting the cells normally interact with this chemical and that it might be one of the factors that stimulates their production. So, she decided this would be a good starting point.
In early tests, she found that norepinephrine, along with other stem cell growth promoters, caused the umbilical stem cells to convert, or differentiate, into oligodendrocytes. However, that conversion only went so far. The cells grew but then stopped short of reaching a level similar to what’s found in the human nervous system.
Davis decided that, in addition to chemistry, the physical environment might be critical.
To more closely approximate the physical restrictions cells face in the body, Davis set up a more confined, three-dimensional environment, growing cells on top of a microscope slide, but with a glass slide above them. Only after making this change, and while still providing the norephinphrine and other chemicals, would the cells fully mature into oligodendrocytes.
“We realized that the stem cells are very sensitive to environmental conditions,” Davis said.
Medical Potential
This growth of oligodendrocytes, while crucial, is only a first step to potential medical treatments. There are two main options the group hopes to pursue through further research. The first is that the cells could be injected into the body at the point of a spinal cord injury to promote repair.
Another intriguing possibility for the Hickman team’s work relates to multiple sclerosis and similar conditions. “Multiple sclerosis is one of the holy grails for this kind of research,” said Hickman, whose group is collaborating with Stephen Lambert at UCF’s medical school, another of the paper’s authors.
Oligodendrocytes produce myelin, which insulates nerve cells, making it possible for them to conduct the electrical signals that guide movement and other functions. Loss of myelin leads to multiple sclerosis and other related conditions such as diabetic neuropathy.
The injection of new, healthy oligodendrocytes might improve the condition of patients suffering from such diseases. The teams are also hoping to develop the techniques needed to grow oligodendrocytes in the lab to use as a model system both for better understanding the loss and restoration of myelin and for testing potential new treatments.
“We want to do both,” Hickman said. “We want to use a model system to understand what’s going on and also to look for possible therapies to repair some of the damage, and we think there is great potential in both directions.”
Besides Hickman and Davis, the other authors on the paper were Xiufang Guo, Stephen Lambert, and Maria Stancescu, all from the University of Central Florida.