A UCF cancer researcher is discovering ways that the body’s own natural killer (NK) cells can be energized to fight deadly pediatric cancers and improve immunotherapy by unleashing the power of our immune system.
UCF Associate Professor of Medicine Alicja Copik has focused her career on developing technologies that “beef up” the body’s NK cells. These cells are the body’s first line of defense in protecting you from viral and other pathogenic infections and even malignancies. Copik’s lab has used nanoparticle technology and genetic engineering to make these cells into better-armed cancer killers.
Her technology is being used to grow NK cells that are in clinical trials for the treatment of adults with leukemia. In recent publications, she has studied if removing one of molecular “brakes” that cancer cells use to avoid being killed — either through antibodies or genetic engineering — can enhance NK cell anti-tumor power. In initial laboratory testing, this approach is showing strong results in killing neuroblastoma cancer cell lines, the most common cancer in infants. Children with high-risk neuroblastoma have a five-year survival rate of just 50%.
These children must undergo painful treatments that include chemotherapy, antibody therapy and bone marrow transplants — half of which fail.
“We throw everything but the kitchen sink at these kids and still can’t stop the cancer,” says Brian Tullius, a U.S. Navy veteran, former flight surgeon, pediatric cancer specialist at AdventHealth in Orlando and the hospital’s research medical director for pediatric cellular therapy, who is collaborating in Copik’s research.
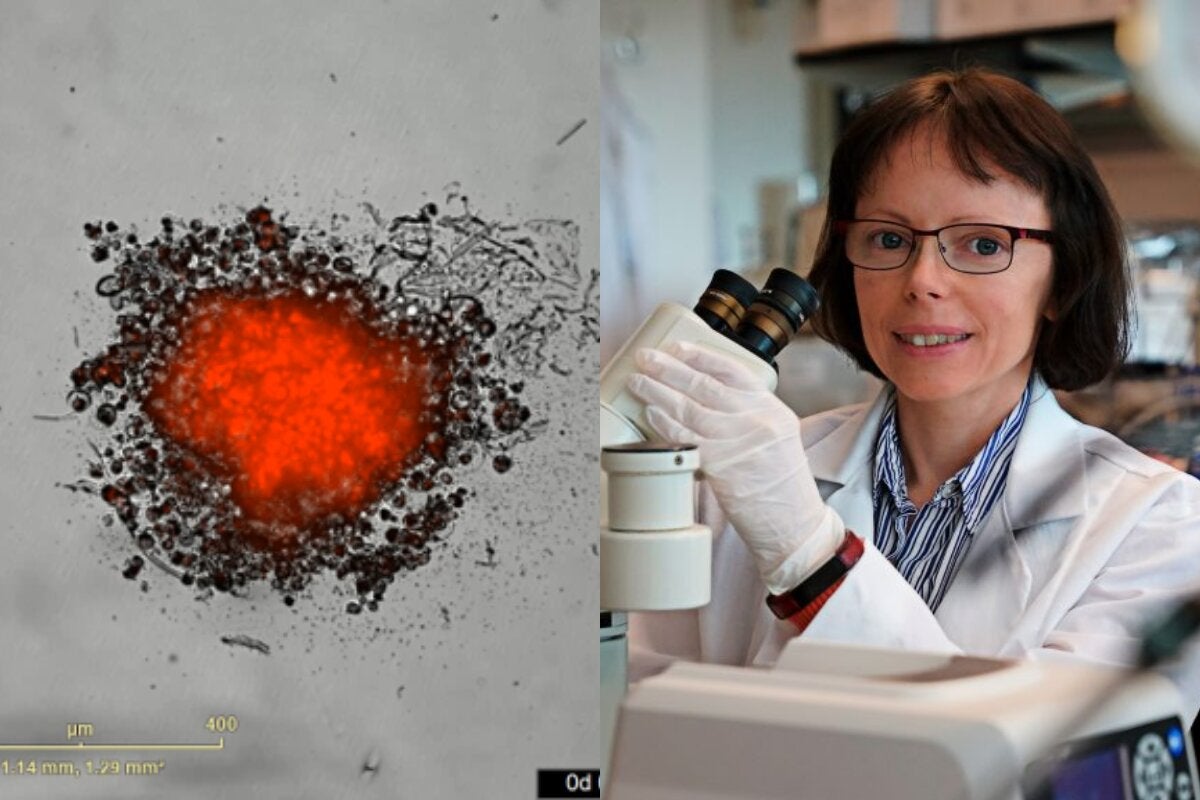
A video from Copik’s lab shows the dramatic results of her technology. Neuroblastoma tumor cells are labeled red. Energized NK cells, which resemble black dots, are added to the red tumor spheroid and quickly kill the tumor cells, as seen by the loss and dispersion of the red cells.
NK cell therapy holds promise for all cancer patients — but especially children with neuroblastoma — because it comes with very few side effects. And NK cells can be donated by a patient’s family, friends or even complete strangers without the new cells attacking the recipient’s healthy cells, which happens with other stem cell transplants or T cell therapies.
Copik is joined by UCF postdoctoral researcher Tayler Croom Perez ’10 in the pediatric cancer study. Their research is supported by the Florida Department of Health Live Like Bella Pediatric Cancer Research Initiative. Croom Perez recently shared the team’s preliminary results with other researchers, physicians and patients at the annual Live Like Bella Pediatric Cancer Research Symposium in South Florida.
Croom Perez received her bachelor’s in forensic science from UCF and completed her doctoral degree at Penn State University. She returned to her alma mater to do NK cell research.
“I have always loved scientific discovery,” Croom Perez says. “Now I have a chance to use my science for translational outcomes that directly affect patient outcomes.”
In the most recent report published by the British Medical Journal, Copik showed that her energized NK cells may improve the performance of cancer immunotherapy treatments that are currently under development. Such treatments work by unleashing the power of our immune system to fight cancer.
Many of the successful therapies block specific molecules, such as PD-L1, that stop our immune system from eliminating tumor cells. However, many of these therapies only work for a small portion of patients. So scientists are looking for other molecules that cancer may use to hide itself from being attacked by immune cells. One of such promising molecules for developing new treatments is called TIGIT (T cell immunoreceptor with Ig and ITIM domains). Initial preclinical and early clinical research studies of TIGIT therapies showed promise. They greatly improved outcomes for patients being treated with currently approved immunotherapies and extended the immunotherapy benefits of these therapies to even more patients.
However, interim results of phase three clinical trials of patients with lung cancer have so far not delivered on the therapy’s initial promise. This has prompted scientists to search for why these TIGIT drugs could be failing and to identify alternative therapeutic strategies.
Copik believes NK cells might be a solution to the challenges faced by TIGIT-targeted therapies. NK cells are critical to the efficacy of immunotherapies, including those targeting TIGIT, and the UCF researcher’s published results suggest that TIGIT therapies may not have worked well because some of them can destroy NK cells. In a prior work funded by the Florida Department of Health James and Esther King Biomedical Research Program and conducted by former postdoctoral student Faqrul Hasan, Copik’s team reported that functional, highly activated NK cells that are better at killing cancer also have a high number of TIGIT molecules on their surface. Since most of the therapeutic TIGIT antibody candidates bind to TIGIT and also mark those cells for destruction by the immune system, including by NK cells, the team hypothesized that activated NK cells may also be eliminated.
The scientists tested this hypothesis in the lab and found that when NK cells have TIGIT antibodies attached to their surface, the NK cells commit fratricide, killing each other off. The UCF scientists found that the fratricide effect could be prevented by genetically engineering NK cells to remove their TIGIT molecules. The team thinks that the destruction of NK cells may be a potential reason why some of the anti-TIGIT candidates have not been performing as expected in clinical trials. This work was performed in collaboration with physician and Professor of Pediatrics Dean Lee and his team at Nationwide Children’s Hospital. The collaborative team also found that NK cells that were genetically modified to lack TIGIT were also more metabolically “fit” and better at killing cancers. The team has shown that getting rid of the TIGIT “brake” on NK cells makes them better cancer killers, even without introducing other immunotherapy drugs.
Copik says the goal of her research is to “try to outsmart cancer.”
“But we have learned that nature is devilishly smart,” she says. “We are hoping that by studying how tumors and immune cells respond and evolve after drug treatments, we will be able to devise better combination treatment strategies to improve outcomes for cancer patients.”