As Breast Cancer Awareness Month begins, two College of Medicine cancer researchers have received statewide grants to support their innovative projects to fight a disease that strikes one in eight American women.
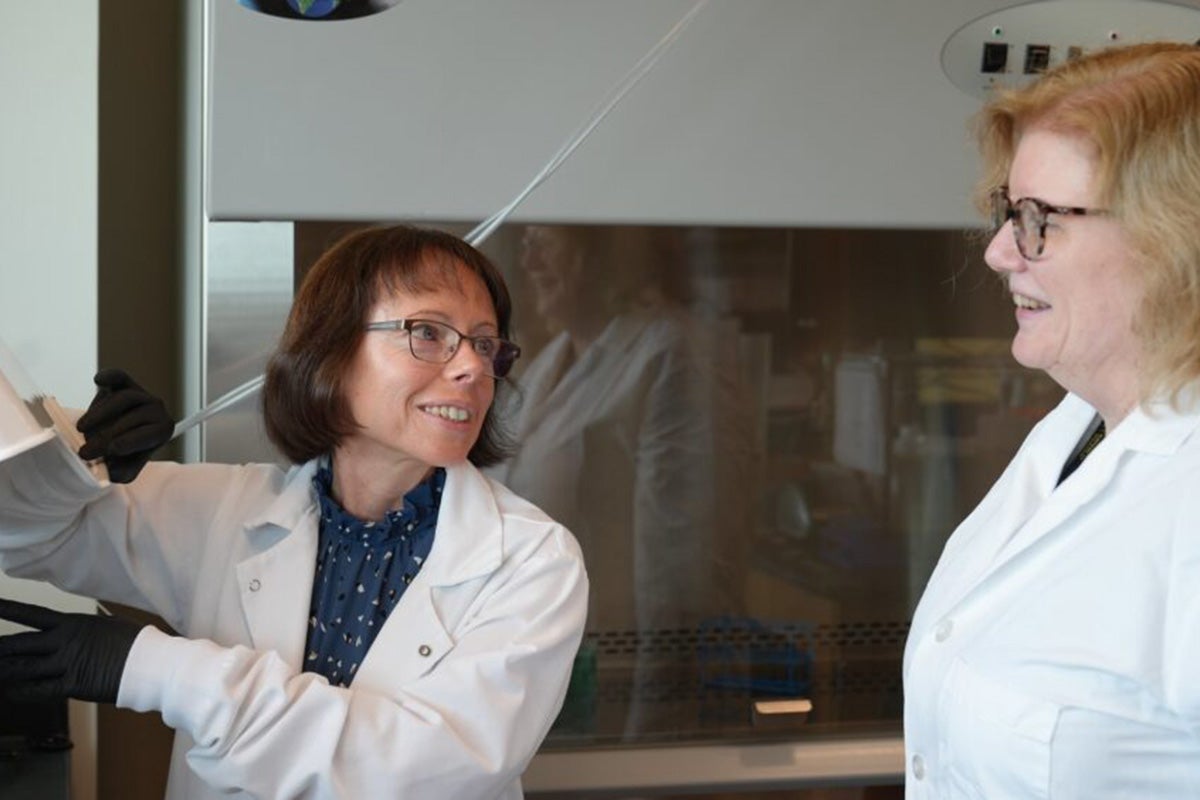
Alicja Copik and Debbie Altomare each received $100,000 from the Florida Breast Cancer Foundation (FBCF), a group focused on supporting innovative research that will create new and better ways to diagnose, treat and perhaps cure the disease.
October is Breast Cancer Awareness Month, dedicated to promoting awareness, screening and prevention of the disease.
Annette Khaled, who leads the College of Medicine’s Cancer Research Division, noted that UCF competed with older, larger programs such as the University of Miami, the Moffitt Cancer Center and the University of Florida to earn the funding. Khaled received UCF’s first FBCF grant in 2012 and since then, seven College of Medicine faculty researchers have earned funding totaling almost $1 million. This is the first year two College of Medicine cancer researchers have earned the state cancer support in the same year.
“This shows we have tremendous intellectual capital in cancer research,” Khaled says. “FBCF is looking for new, innovative ideas in fighting breast cancer and they are supporting UCF.”
Copik focuses her research on better arming the body’s natural killer (NK) cells to wipe out cancer. NK cells are the first line of defense in warding off pathogens, such as viruses. Through genetic engineering and nanoparticle technology, Copik has developed NK cells that are better at recognizing and killing cancer cells. Such therapies are much easier on patients. NK cells can do their work without the debilitating impact that comes with current cancer treatments like chemotherapy and radiation. And these energized NK cells can be donated to cancer patients from complete strangers without a risk of rejection.
The FBCF grant will help Copik refine her technologies to specifically fight breast cancer. She will also study how the most recent and still experimental treatment strategies against metastatic breast cancer may affect patients’ own NK cells. Because NK cells clear any residual tumor cells in the body, it’s important that new treatments don’t deplete the body’s natural fighters. With this knowledge, scientists can design better clinical trials and create more combination therapies that incorporate NK cells as additional cancer fighters.
“We need to harness innovation and innovative thinking to improve care.” — Alicja Copik, associate professor of medicine
Copik’s NK therapies are currently in clinical trials. She is also researching whether removing one of molecular “brakes” that cancer cells use to avoid being killed — either through antibodies or genetic engineering — can enhance NK cell anti-tumor power. In initial laboratory testing, this approach has shown strong results in killing neuroblastoma cancer cell lines, the most common cancer in infants.
“We need to focus on the quality of life for metastatic breast cancer patients,” she says. “We know chemo and radiation work, but they have drastic side effects. We need to harness innovation and innovative thinking to improve care.”
Altomare has vast experience in cancer biology. Her focus is on the cellular pathways that can signal cancer cells to grow or help immunity cells better fight the disease. She is examining the role that inflammation plays in pancreatic cancer — one of the deadliest forms of the disease — and harnessing the body’s innate immunity to create new therapeutics for ovarian cancer.
One of the challenges of breast cancer research is the heterogeneity of breast tumors — meaning one patient may have a variety of cells in their tumor that is different from other patients. That makes it difficult for researchers and physicians to determine what exact molecular alternations occurred to cause the cancer and prescribe individualized treatments.
Altomare’s lab at the College of Medicine has been studying a particular growth factor called FGFR4 (fibroblast growth factor receptor 4) in breast cancer cells. Her work has discovered that while encouraging the growth of cancer cells, the growth receptor may also suppress immune cells.
She will use the FBCF funding to examine how the presence and absence of the growth factor and pathways in specific tumors impact their ability to spread and how they impact immunity. Her hope is that the discoveries will help create new metastatic breast cancer therapies.
“We’re looking at ways the tumor cells can be reprogramed to better react to therapies and not be so drug resistant,” she says.
The College of Medicine’s Cancer Research Division, housed in the Burnett School of Biomedical Sciences, focuses its work on a variety of areas, including how patients’ genes play a role in their cancer risk, what causes cancer and cancer metastasis and discovering new ways to harness the body’s immune system to fight cancer.