College of Medicine researchers are developing a more effective way to treat glioblastoma — an aggressive, incurable form of brain cancer. Patients currently live just 12 to 15 months after diagnosis despite surgery, radiation and chemotherapy.
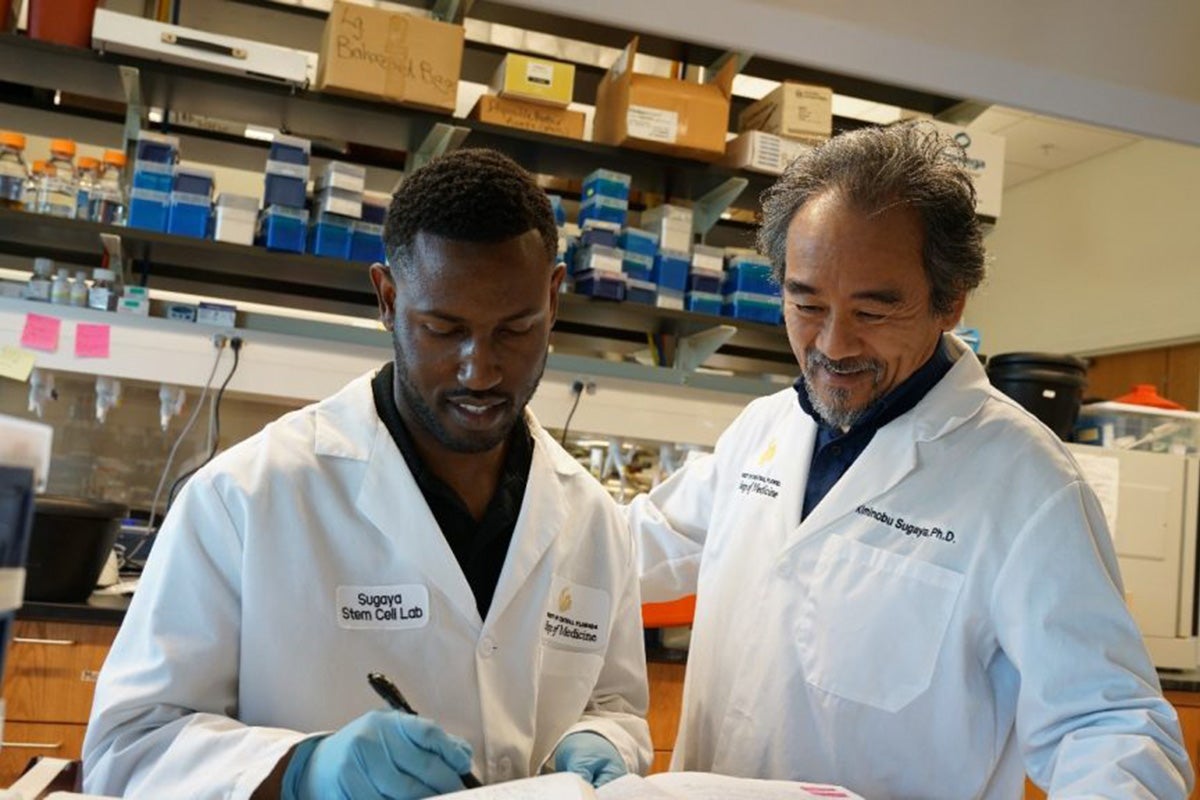
New research led by Kiminobu Sugaya, a stem cell researcher and neuroscientist at UCF’s Burnett School of Biomedical Sciences, found that targeting a drug resistant mechanism in cancer stem cells significantly enhanced the efficacy of traditional cancer therapies — making them four times more effective against glioblastoma. Current FDA-approved drugs kill less than 25% of glioblastoma cancer stem cells (CSCs).
These cells are a subpopulation of cancer cells that are highly resistant to current therapies. Scientists theorize that cancer returns and spreads because CSCs remain in the body. That’s why they are exploring ways to kill them outright.
“Cancer stem cells are bad stem cells that are programed to become a cancer,” Sugaya says. “They withstand cancer therapies, raise their ugly head, regrow and metastasize.”
Sugaya’s team developed a new drug delivery system by creating a technology that destroys the RNA, or ribonucleic acid, that the stem cells use as a blueprint to produce proteins. This unique strategy inhibits the expression of embryonic stem cell genes that are pivotal in CSC’s drug resistance. And because embryonic stem cell genes are not expressed in normal adult cells, this breakthrough approach reduces potential for side effects in healthy cells.
Jonhoi Smith is a doctoral student under Sugaya and the first author on their research paper published in the journal Genes. He said the treatment could increase life expectancy for glioblastoma patients.
“This treatment could be a precious gift for glioblastoma patients. When I think about the loved ones I’ve lost in my life — my father, my grandmother — I often wish I could have had more time with them,” he says. “The idea of offering the potential of a whole new life to people who are facing a death sentence in less than a year means a lot to me.”
One of the significant challenges in treating glioblastoma is effectively delivering treatments to the brain. That’s because the brain is protected from external germs and substances by the blood-brain barrier, which can also prevent treatments from reaching brain tissues.
To overcome this obstacle, Sugaya’s therapy is based on exosomes, nano-sized particles with a lipid membrane that are naturally produced by cells. Exosomes function as cellular communicators, transporting proteins, lipids and genetic material between cells, thereby influencing a wide array of biological processes and functions. Their efficiency in carrying molecules across various parts of the body has inspired scientists to investigate exosomes as potential drug delivery vehicles.
“Many current drug delivery systems, including viruses, may cause side effects,” Sugaya explains. “We’re using the body’s natural delivery systems and have developed technologies to modify them to carry therapeutic molecules with targeted delivery to specific tissues.”
Marvin Hausman is CEO of Exousia AI, the company that is funding the glioblastoma exosome preclinical research. He heard about Sugaya’s lab and says that when he visited the lab at UCF’s Academic Health Sciences Campus in Lake Nona, he was inspired by its capacity for innovative discoveries.
“I have thoroughly analyzed this exosome-based targeted drug delivery system many times, and the potential that this unique technology offers.” Hausman says. “We are embarking on a revolutionary new development in medicine.”
Thanks to funding from Exousia AI, the research is advancing to mouse models carrying human glioblastoma, with preliminary results expected as early as this summer.
Sugaya has dedicated more than 40 years to neuroscience research focused on Alzheimer’s disease, with an emphasis on stem cells for the last 26 years. He moved to the U.S. after receiving his doctoral degree from the Science University of Tokyo in 1988. He joined UCF as a professor in 2004. His cancer research began in 2010 when he discovered stemness gene expressions, the self-renewing and differentiating property that allows stem cells to grow and spread, in CSCs. He is recognized as an expert in the field of exosome research and recently received Florida Innovation Funding from the State Department of Health for his studies.