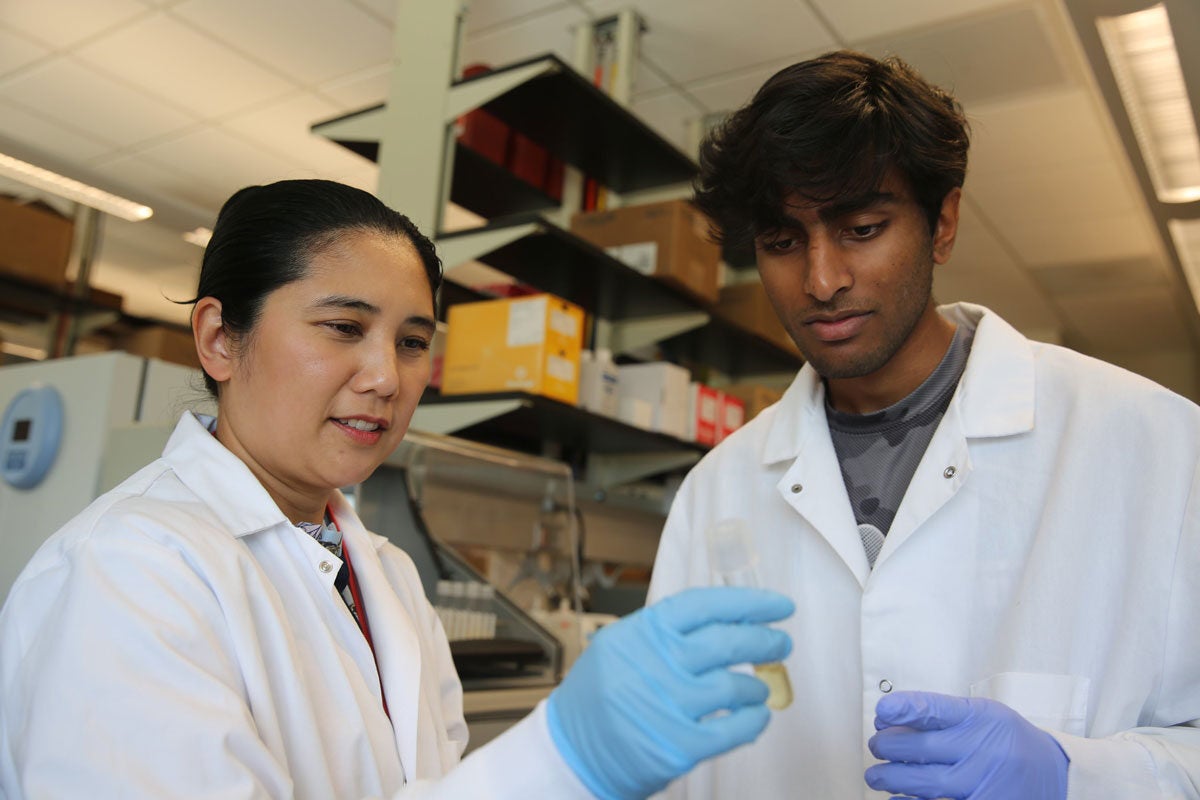
For those suffering from allergies, especially allergic asthma, springtime can be dreadful. Fortunately, UCF researcher Justine Tigno-Aranjuez is making breakthroughs that could one day make many common allergies a thing of the past.
For years, research and therapies for allergic asthma have been focused largely on targeting the inflammatory cytokines in the body that react to allergens and cause overproduction of mucus, wheezing and difficulty breathing. Commonly prescribed drugs like Omalizumab, Dupilumab, Mepolizumab and Reslizumab lower or block the various cytokines and antibodies responsible for the asthmatic response, but they work after a patient’s airway inflammation is well underway.
Tigno-Aranjuez wanted to find a new approach to keep allergen receptors from reacting in the first place. So she utilized a technique called LRC-TriCEPS — which identifies receptors in cells — for a common allergen, house dust mite. The technology showed a cell protein called LMAN1 that had never before been recognized for having a role in the body’s allergen response.
Her findings were recently published in Cell Reports, her highest impact paper to date.
“When we first had this discovery, we wanted to know, ‘What is this protein? What is already known about LMAN1 as an allergen receptor?’ and the interesting thing was that people had not been paying much attention to this protein in the context of allergy or allergic asthma,” she says.
Before her discovery, LMAN1 was generally known as a cargo receptor — a protein that transports other proteins inside and outside the cell. However, Tigno-Aranjuez demonstrated that house dust mite allergens and LMAN1 can bind together on the cell surface to cause the inflammatory or allergic reaction. Her research further showed that the binding depended on specific mannose sugar structures on the house dust mite allergens. This discovery has tremendous potential since many other common allergens, including pollen and fungi, are mannosylated, or modified by the addition of mannose sugars.
“Our thinking is that this could potentially not just be restricted to dust mites because many other allergens are mannosylated, this could be a very broad receptor that recognizes many different allergens,” she says. “If you are thinking in terms of potential therapy, by understanding how LMAN1 recognizes dust mites and the consequences of such recognition, you could apply this to many other settings, and that is what we are currently trying to explore.”
The National Institutes of Health also saw potential with the UCF research, having just awarded Tigno-Aranjuez a $1.5M R01 grant to see if LMAN1 has a role in the expression of other mannosylated allergens.
Tigno-Aranjuez’s research on LMAN1 is performed in collaboration with the Cleveland Clinic. Bin Zhang, associate professor at the Lerner Research Institute, serves as co-investigator on this study. Zhang is considered an expert in LMAN1.
“LMAN 1 has been largely known as a protein that is involved in transporting proteins from inside cells to the outside of cells,” Zhang says. “This research is the first one to show an entirely new function of LMAN1, as a receptor to bring proteins, such as allergens, from outside of cells to the inside. This could open up a new pathway for treatment.”
With hundreds of thousands of allergic asthma cases in the United States every year, and many more worldwide, this research represents a step forward toward helping these patients.
“Asthma is so prevalent that sometimes, people think, ‘We’ve already got a lot of treatments, we’ve got it covered.’ The reality is that we could always use more options, we could always improve upon existing treatments,” Tigno-Aranjuez says. “Many treatments can only be prescribed if you meet certain clinical criteria, many treatments are cost prohibitive, many are not covered by insurance. So any new treatment we can put forth that could potentially be a more universal treatment would always be an advance.”
Tigno-Aranjuez and her team are now conducting research to confirm their hypothesis that other mannosylated allergens, such as pollen, are also recognized by LMAN1. If true, this could have broad implications in future therapies for many of the most common allergens.
Tigno-Aranjuez immigrated to the United States from the Philippines to conduct her graduate and postdoctoral training at Case Western University in Cleveland. She joined UCF in 2015 and focuses her research on immune signaling pathways involved in chronic inflammatory diseases such as asthma and Crohn’s disease.