Patient Simulation: The Future of Educating Future Nurses
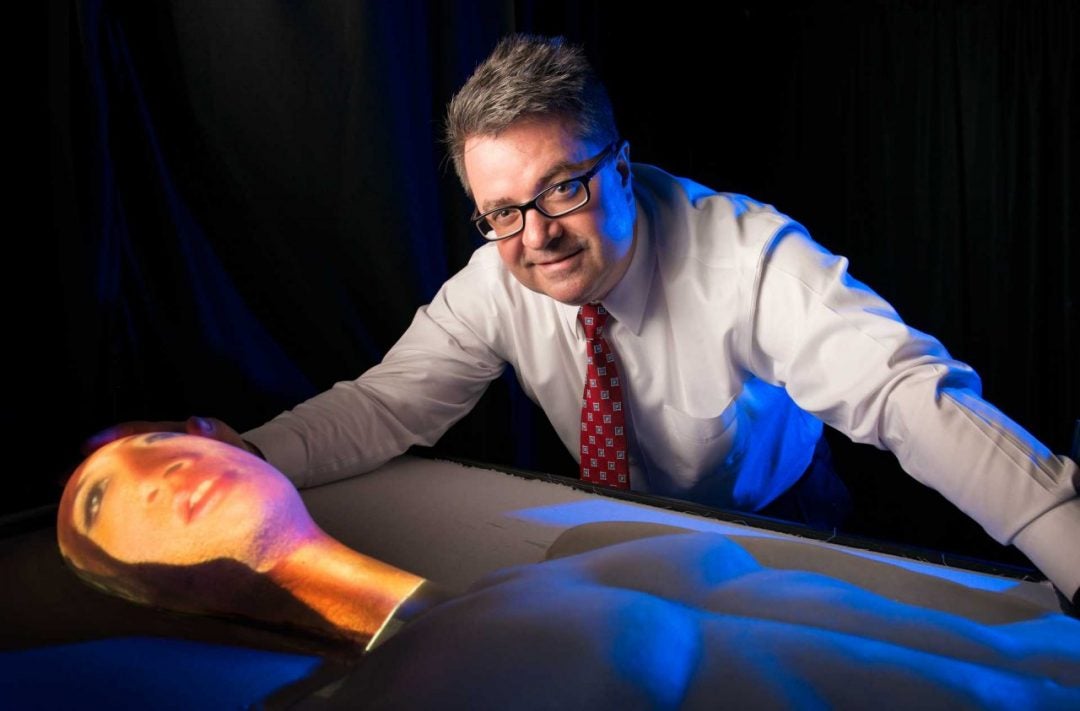
Dr. Gregory Welch, AdventHealth Endowed Chair in Healthcare Simulation at the University of Central Florida’s College of Nursing, and UCF students and faculty colleagues have come up with a new kind of patient stand-in, one that melds the physicality of a mannequin with the versatility of virtual humans.
The results of their work, two prototypes of physical-virtual pediatric patient simulators, could elevate nursing education to new heights.
Welch, whose background is in hardware and software engineering, is also a professor of computer science, modeling and simulation. While he began the development of the physical-virtual patient seeking to develop an adult simulator, he later decided to focus on pediatric prototypes because of the difficulties that exist in educating students to diagnose and treat children.
“For adults, you can actually leverage professional human role players to serve as patients. You can’t do that with children,” Welch says. “You can’t hire a 5-year-old to pretend to be sick. As such you are limited to mannequins that are relatively static in their appearance and behavior. There’s really a need for something that’s more ‘alive’ than a piece of rubber to interact with.”
The pediatric prototypes developed at UCF are fitted with digital light projectors that can beam the image of a child from below onto a child-shaped physical form. The result is a physical-virtual patient that can appear to breathe, cough, blink and squirm. They wince in pain when pricked with a needle and smile at a nurse’s joke. Temperature controls allow for simulation of a fever and cooling of the extremities. A nurse can place a real stethoscope on the body to hear wheezing in the chest, gurgling in the stomach and other internal sounds of the body.
“We can make the patient speak, see the lips move,” Welch says. “We are working on the ability to make the child autonomously aware so that when you walk up to the child, we want the child to naturally turn and look at you.”
Having an interactive, human-like patient has the potential of vastly improving a trainee’s opportunities to safely practice the patient interactions involved in the diagnosis and treatment of disease, Welch says.
“We are trying to get closer to reproducing the appearance and complete set of signals that a patient sends — speech, sounds and facial expressions,” he says. “Diagnosing a patient is very dynamic, tactile, hands-on and fluid. You are watching the patient, you are asking questions, judging everything they say and everything they do. For example, subtle nonverbal patient behaviors resulting from a question could indicate there is more going on than the patient is telling you.”
The UCF innovation has potential for being cost effective as well. Traditional mannequins can be expensive and don’t allow changes in their physical appearance. In contrast, physical-virtual patient simulators can take on nuanced personas depicting people of different races, ethnicities and genders with a variety of disease symptoms.
The Birth of an Innovative Way to Learn How to Treat Patients
For Welch, the idea for physical-virtual avatars began to germinate more than 15 years ago during a conversation at the Pentagon with a physician-turned-administrator. The administrator expressed a longing to go back to practicing medicine. He wondered about the possibility of creating a physical robotic persona of himself that would allow him to be with patients without leaving his Pentagon office.
Welch’s first reaction was that the scenario belonged in the pages of a sci-fi novel. But the more he thought about it, the more intrigued he became by the idea of developing a physical-virtual persona.
“Then I had this idea out of the blue that you could actually use computer graphics and projected imagery to present the appearance of that exact physician on a physical form like a robot,” he says.
Welch also brainstormed ideas with the director of a burn center on how physical-virtual avatars could help burn victims, who are often isolated to avoid risks of infection. They came up with a scenario where a homebound burn patient could sign up for a mobile physical-virtual avatar in a mall, project his or her own image on the avatar, and browse store racks, visit cafes and chat with salespeople.
“It would offer a way for them to re-engage with society in a very safe and gentle way,” he says.
When Welch came to UCF, his office happened to be right across from the College of Nursing. In his conversations with nursing faculty, he began to understand the challenges and needs in nursing education. He learned about the role of mannequins in how nursing students gain knowledge and patient-care skills. It struck him that the ideas that had long simmered in his mind could be used to develop a new kind of patient stand-in.
The Next Generation of Nursing Simulation
Welch and UCF colleagues are working on adding touch sensing and other enhancements to the pediatric prototypes. The next step is the experimental use of the physical-virtual avatars in regional hospitals with professional nurses and doctors. Among other things, Welch wants to explore how physical-virtual patients can help students become better trained in the diagnosis of disease in patients of different racial and ethnic backgrounds. He is also interested in using patient simulators to study how implicit biases can affect patient care.
Beyond the experimental stage and in the longer term, Welch expects to see widespread use of physical-virtual patient simulators in conjunction with mannequins and other learning aids.
“In five to 15 years, my vision would be to start seeing physical-virtual patient simulators in existing simulation centers throughout the country and throughout the world as a complement to the other tools we have to train people.”
UCF’s Online Healthcare Degrees
- Autism Spectrum Disorders
- Chemistry, MS - Forensic Science
- Executive Master of Health Administration, EMHA
- Fundraising
- Gender Studies
- Health Informatics and Information Management, BS
- Health Informatics, BS
- Health Services Administration, BS
- Healthcare Simulation
- Healthcare Systems Engineering Certificate
- Healthcare Systems Engineering, MS
- Integrative General Studies, BGS
- Interdisciplinary Studies, BA/BS
- Master of Public Administration, MPA
- Master of Science in Healthcare Informatics
- Master of Social Work Online
- Nonprofit Management
- Nonprofit Management, MNM
- Nursing Education
- Nursing Practice, DNP, Advanced Track
- Nursing Practice, DNP, Executive Track
- Nursing, BS
- Nursing, BSN to PhD
- Nursing, MSN
- Nursing, PhD
- Project Engineering
- Psychology, BS
- Public Administration
- Research Administration Certificate
- Research Administration, MRA
- Systems Engineering







